
Abstract:
Calcium is a very abundant mineral that is essential for bone formation, muscle contraction, and hormone functioning. Calcium needs do not increase during pregnancy but if adequate amounts are not obtained, the mother’s calcium stores may become depleted and her bones weakened in order to provide the growing fetus with proper amounts. Food, and particularly dairy, is an ideal source of calcium. If you avoid dairy, make an extra effort to include alternative dietary sources of calcium in your diet every day, including chia seeds, green vegetables (kale and bok choy), almonds, sardines and salmon. Unless you are averse to all these foods or have another medical issue that necessitates supplementation, a calcium supplement, beyond a prenatal, is not necessary. If you have high blood pressure or are at risk for preeclampsia, some studies have found benefits from calcium (and magnesium supplementation).
What is Calcium? Why Do I Need It?
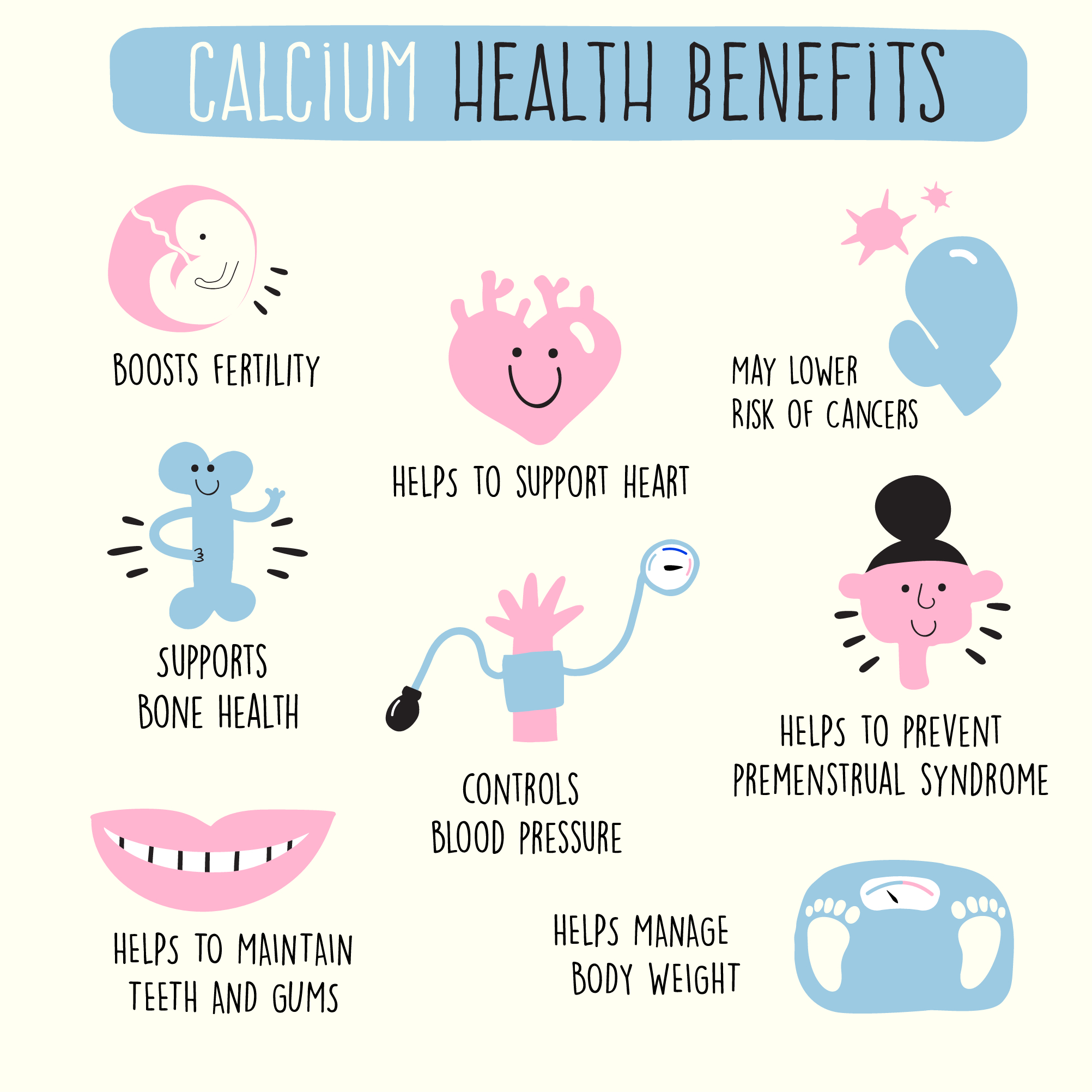
Calcium is the most abundant mineral in the body and is essential for a variety of bodily functions including muscle contraction, bone formation, enzyme function, and hormone signaling. The ionized pool of calcium in our body’s circulatory system, extracellular fluid, and various tissues mediates all of calcium’s functions; blood vessel contraction and dilation, muscle function, blood clotting, nerve transmission, and hormonal secretion. Calcium is needed to keep our bones strong and healthy. Almost all (98%) of calcium in the body is stored in the bones, and the body uses the bones as a reservoir for, and source of, calcium to maintain calcium homeostasis. This occurs through a process called bone remodeling, which involves constant resorption and deposition of calcium into new bone. Bone remodeling is required to change bone size during growth, repair damage, maintain serum calcium levels, and provide a source of other minerals. The body naturally maintains a tight range of serum calcium, however, adequate intake of calcium and vitamin D does greatly influence growth and peak bone development. Genetics and exercise are other factors, however, nutrition allows a given genetic potential for healthy bones to be fully expressed.
What About Calcium and Pregnancy?
Even though the amount of calcium needed during pregnancy does not increase, making, sure enough, calcium is obtained becomes more critical, especially during the second and third trimesters of pregnancy. During this time, your baby’s bones and teeth are growing immensely and require a continuous supply of calcium. A series of physiological changes occur in mom during pregnancy related to calcium metabolism:
- Falling albumin (a carrier protein that helps keep fluid in your bloodstream) level
- Expansion of extracellular fluid volume resulting in hemodilution
- Increase in kidney function
- Placental calcium transfer
The body also naturally responds to calcium needs during pregnancy by increasing intestinal calcium absorption rates. However, the growing fetus will take all the calcium it needs from the mother’s personal calcium stores and deplete them, weakening bones in the process, if they are not replenished properly and intake is not adequate. Women begin to lose bone mass in their 30s and they’ll lose it faster if calcium is drained from their own bones to help build baby’s. Getting calcium daily, especially during pregnancy, also helps prevent osteoporosis later in life. Inadequate calcium also increases the risk for pregnancy complications like preeclampsia, preterm delivery, low birth weight, and postpartum hemorrhage whereas adequate calcium intake can help prevent the development of high blood pressure.
Studies have also shown that your calcium intake during pregnancy may affect the health and strength of your baby’s bones later in life. One study found a link between higher maternal calcium intake and a child’s body bone mass (one of the indicators of bone health) at age nine, suggesting the potential effects of calcium intake during pregnancy on the child’s bone development later in life.
What Is Needed for the Body to Optimally Process Calcium?
Thank you biology for automatically increasing calcium absorption rates during pregnancy. Much appreciated! It should also be noted that calcium absorption varies by type of food. The absorption of calcium from dairy products and fortified foods is about 30%. However, certain compounds in plants, like oxalic acid and phytic acid, decrease calcium absorption by forming insoluble salts with calcium. Thus, spinach (along with other plant foods like collard greens, sweet potatoes, rhubarb, and beans) has only a 5% absorption rate, whereas milk has a 27% absorption rate. The bioavailability of calcium from other plants that do not contain oxalic and phytic acid, such as broccoli, kale, and cabbage, is similar to milk. Although, the amount of calcium per serving in these plant foods is much lower. Calcium absorption rates can also be impacted by caffeine and phosphorus intakes, and to a greater exten by low status of vitamin D. *Caffeine can act as a diuretic causing increased urination. An increase in urination may cause some calcium to leave your body. This loss should be very minimal, however, if you stay within the recommended guidelines for caffeine (approximately one 12 ounce cup of coffee per day) during pregnancy.
It is fairly easy to get adequate amounts of calcium from dietary sources, particularly if the diet includes dairy products. However, what is seen more often than low calcium intake is inadequate consumption of complementary nutrients such as vitamin D, vitamin K2 and magnesium. These nutrients are required for your body to optimally process calcium and build strong bones.
How Should I Get It?
Food is ideal, but sometimes a supplement can be helpful. If you think you’re falling short or have a hard time getting enough calcium from your diet, talk to your doctor about adding a supplement. A recent review of studies on prenatal calcium (involving 15,730 women) showed that calcium supplementation led to a decreased risk of high blood pressure, preeclampsia, severe eclampsia, and preterm birth, and an increase in baby birth weight. But only for those women with low dietary intakes of calcium. If your dietary intake is adequate, you likely don’t need a supplement, and studies show no effects on the baby’s bone mineral mass with calcium supplementation in women who already have adequate calcium intake. Note: If you choose to take a calcium supplement at the direction of your healthcare provider, be aware that calcium and iron compete for absorption. This can be a problem for many women who enter pregnancy with low iron status. Take your calcium at a separate time from an iron supplement.
Ok, what is the best form of calcium supplement?
The most common forms of calcium in supplements are calcium carbonate and calcium citrate. Calcium carbonate supplements tend to be the best value, because they contain the highest amount of elemental calcium (about 40% by weight). However, this form also requires stomach acid for absorption and should be taken with food. Most people tolerate this supplement well, but some people complain of mild constipation or feeling bloated as a side effect. Calcium citrate is less dependent on stomach acid for absorption than calcium carbonate, so it can be taken without food.
The supplement dicalcium malate is a compound of calcium and malic acid. This form is easier to absorb than calcium alone. It also contains a small amount of vitamin D to aid in absorption. Dicalcium malate can be consumed with or without food and is recognized as a calcium source that does not increase the risk of kidney stones, and in fact it protects against stone-forming potential. The only downside to this supplemental form is its higher cost compared to other sources of calcium commonly used in supplements or fortified foods.
How Much?
The RDA for women during pregnancy is 1g (1000 mg) per day. There are some conversations, including those by the World Health Organization, that recommend a calcium dose of 1.5 g to 2 g during pregnancy for women with low dietary calcium intakes. Women with low calcium intakes should either increase their intake of food sources of calcium, such as milk or cheese or add a supplement that provides around 600-1000 mg of calcium per day. Women with lactose intolerance need careful assessment of their calcium intake because they tend to drink little milk and have relatively low calcium intakes. Women should also get adequate sunlight exposure and increase their intake of vitamin D supplements.
Am I Getting It From Food?
Yes, many foods contain calcium and are the ideal source of this mineral. Milk, yogurt, and cheese are rich natural sources of calcium. One cup of plain yogurt (415 mg), one slice of swiss cheese (270 mg), and one cup of raw kale (100 mg) can be great additions to your pregnancy diet. What about cottage cheese! There are many non-dairy calcium sources as well, including green leafy vegetables, bok choy, broccoli, almonds, sesame seeds, chia seeds, and sardines or salmon canned with the bones. Even though spinach is abundant in calcium, the calcium is not bioavailable, because it contains oxalic acid, which prevents your body from absorbing it. Most grains do not have high amounts of calcium unless they are fortified. Foods fortified with calcium in the United States include many fruit juices and drinks, tofu, and ready-to-eat cereals.
How Do I Know If I Am Getting Enough?
Total calcium levels can be measured in three different ways:
| Marker | Description |
| Serum calcium levels: | used as a measure of calcium, however, serum levels do not reflect nutritional status because of their tight homeostatic control. Typically 8.8 to 10.4 mg/dL in healthy people. |
| Ionized calcium levels: | a measure of the biologically active (free) form of calcium in the body. Typically 4.6 to 5.3 mg/dL in healthy people. |
Absorptiometry testing of bone mineral density: used to assess cumulative calcium status over the lifetime because the skeleton stores almost all calcium in the body.
Can I Get Too Much? (Toxicity of Calcium)
More is not always better and that is definitely the case with calcium, only a concern if taken in supplemental form. As the upper tolerable limit, an adult female should not take more than 2,500 mg of calcium each day. Ingesting too much calcium can cause constipation, kidney stones, possible trouble absorbing other minerals such as iron and zinc, and irregular heartbeat.
Prenatal Vitamin Brands: What's the Calcium Amount and Type in Popular Prenatal Brands?
| Name of the Prenatal | Amount | Types |
| Parsley Health Prenatal: | 400 mg | (dicalcium malate) |
| Modern Fertility Prenatal: | None | N/A |
| Ritual Prenatal: | None | N/A |
| FullWell Prenatal: | 400 mg | (dicalcium malate) |
| Perelel: 2nd Trimester Prenatal Pack 200 mg (calcium malate):3rd Trimester Prenatal Pack: | 100 mg | (calcium malate) |
| NatureMade Prenatal Multi + DHA: | 150 mg | (calcium carbonate) |
| Seeking Health: Optimal Prenatal: | 400 mg | (dicalcium malate) |
| Designs for Health: Prenatal Pro: | 140 mg | (Dimacal dicalcium malate) |
Prenatal Analysis:
Most of the prenatal vitamins listed above utilize the dicalcium malate form of calcium supplementation, which is a beneficial form that is easy to absorb. Depending on how calcium-rich your diet is, it may be important to select a prenatal vitamin with calcium present. Some prenatals include as much as 400 mg, while others include 150 mg.
Resources:
- Nichols L. Real Food for Pregnancy: The Science and Wisdom of Optimal Prenatal Nutrition. First edition. Lily Nichols; 2018.
- Murkoff HE, Mazel S. What to Expect When You’re Expecting. Fifth edition. Workman Publishing; 2016.
- Avena NM, Fear G. What to Eat When You’re Pregnant: A Week-by-Week Guide to Support Your Health and Your Baby’s Development during Pregnancy. First edition. Ten Speed Press; 2015.
- Hofmeyr GJ, Lawrie TA, Atallah ÁN, Torloni MR. Calcium supplementation during pregnancy for preventing hypertensive disorders and related problems. Cochrane Database Syst Rev. 2018;2018(10):CD001059. doi:10.1002/14651858.CD001059.pub5
- Office of Dietary Supplements - Calcium. Accessed April 27, 2022. https://ods.od.nih.gov/factsheets/Calcium-HealthProfessional/
- Calcium in Pregnancy. American Pregnancy Association. Published March 26, 2015. Accessed April 27, 2022. https://americanpregnancy.org/healthy-pregnancy/pregnancy-health-wellness/calcium-in-pregnancy/
- Kumar A, Kaur S. Calcium: A Nutrient in Pregnancy. J Obstet Gynaecol India. 2017;67(5):313-318. doi:10.1007/s13224-017-1007-2
- How Much Calcium Do You Need During Pregnancy? Verywell Family. Accessed April 27, 2022. https://www.verywellfamily.com/calcium-needs-during-pregnancy-4580491
- Nutrition During Pregnancy. Accessed April 27, 2022. https://www.acog.org/en/womens-health/faqs/nutrition-during-pregnancy
- Choosing a calcium supplement. Harvard Health. Published March 20, 2017. Accessed April 27, 2022. https://www.health.harvard.edu/nutrition/choosing-a-calcium-supplement
- Reinwald S, Weaver CM, Kester JJ. The health benefits of calcium citrate malate: a review of the supporting science. Adv Food Nutr Res. 2008;54:219-346. doi:10.1016/S1043-4526(07)00006-X