
Abstract:
When it comes to Omega-3s and pregnancy, the focus should be on a specific type of polyunsaturated fatty acid, DHA. This nutrient supports the development of the baby's brain, eyes, and nervous system and keeps Mom's brain functioning smoothly and her mood balanced. For a healthy and thriving pregnancy, it is advisable to consume at least 300 mg/day of DHA, which is found in low-mercury fish sources or supplements.
What are Omega-3s? DHA? EPA? And Why Do I Need It?
Ah, omega-3s fatty acids are those essential polyunsaturated fatty acids that are critical to many bodily functions and are only obtained from the food we eat. They are the nutrients that put the gravity on the great pregnancy fish debate. Should I eat it, or should I not? What about mercury?
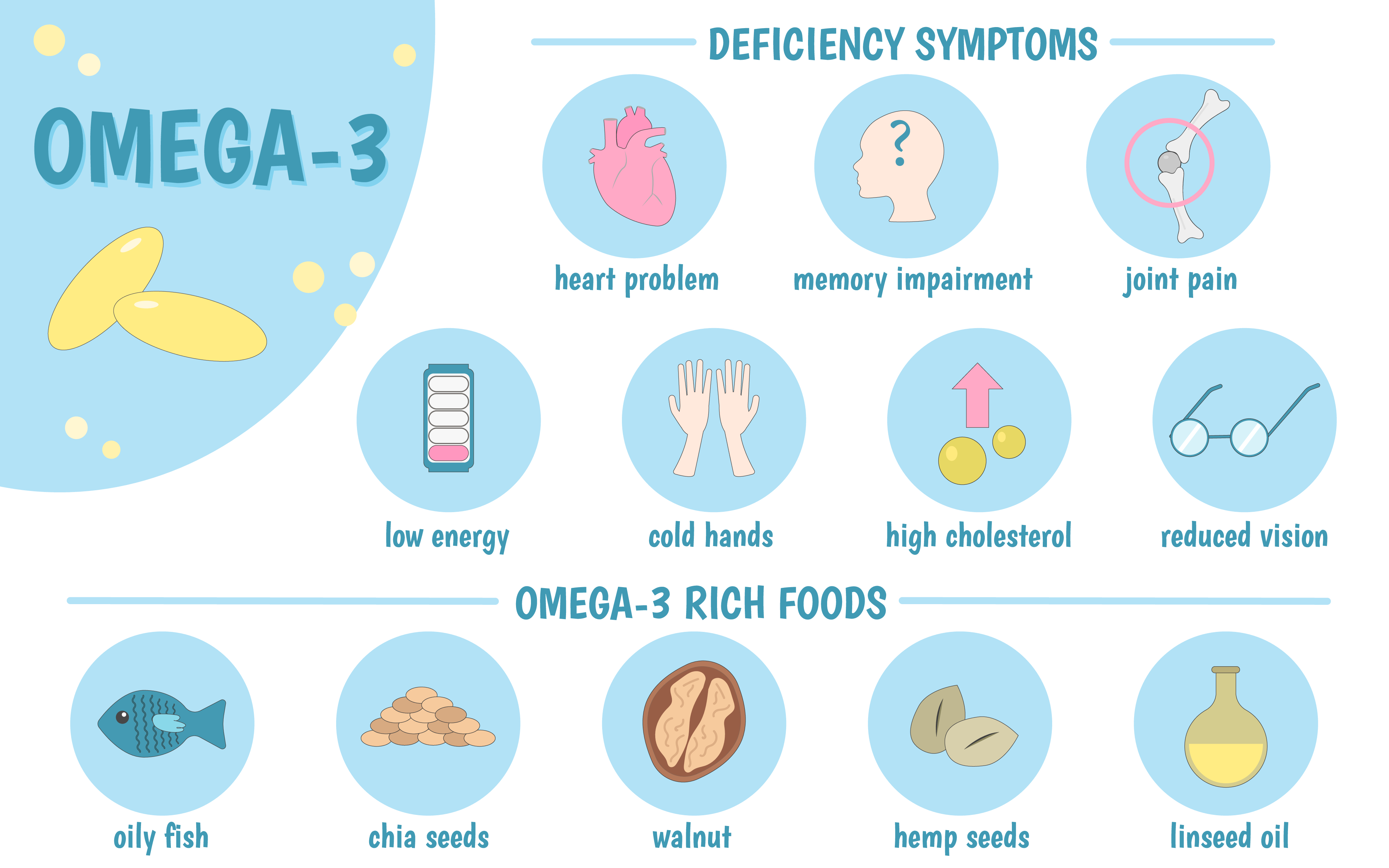
Omega-3s are very important for women during pregnancy and lactation. These fatty acids make up the phospholipids that form the structures of our cell membranes and come in three main types:
-
- DHA (Docosahexaenoic acid): Most Important Fatty Acid - supports the brain, eyes, and central nervous system.
- EPA (Eicosapentaenoic acid): Transport Fatty Acid - Supports the heart, immune system, and inflammatory response. EPA also plays an essential role in helping DHA cross the placenta and nourish the growing fetus.
- ALA (Alpha-linolenic acid): Most Common Precursor Fatty Acid - Found in plant foods, a small percentage is converted into EPA and DHA.
Baby's Development:
A woman's demand for DHA increases during pregnancy and is essential for the proper development of babies in utero and in infancy. DHA/EPAs are essential to support the healthy development of your baby's brain, eyes, and nervous system. DHA is crucial for fetal brain and retina development during the third trimester, as the fetus requires about 50 to 70 mg a day of DHA during that last trimester.
The DHA content of your baby's brain triples during the first 3 months of life, and the fatty acid continues to impact the brain's development post-birth for up to 18 months. Maternal DHA intake affects child development, particularly breastfed babies, as babies accrue DHA into their central nervous systems throughout infancy. Omega-3 fatty acids are also very important for heart health and the development of your baby's immune system.
Full Term Pregnancy and Birth Weight:
Getting enough DHA during pregnancy may reduce the chances of your baby being born too early(pre-term labor) or being born at a low birth weight. DHA and EPA are known for their anti-inflammatory properties and have been shown to produce compounds that control the inflammatory response in the uterus, preventing preterm birth. One randomized controlled trial showed that preterm birth (<37 weeks) and early preterm birth (<34 weeks) were reduced in women receiving omega-3 supplementation compared to those women who did not receive supplementation.
Mother's Memory (Mom Brain):
Circulating DHA concentrations are high in retinal and brain membrane phospholipids, and are involved in your (you, the Mom's!) visual and neural function and neurotransmitter metabolism. It is incorporated into the phospholipid structure of every brain cell, impacting how neuronal signals are sent and received. DHA accounts for ~15% of the fatty acids in your brain. H4: So when pregnancy makes strong demands for this nutrient, a mother's stores can become depleted and her brain activity compromised. Without adequate DHA intake, what is called "mom brain" can result, characterized by reduced cognitive function, depression, and greater susceptibility to stress.
Mother's Mood:
Some research has shown that adequate DHA and EPA intake reduces the risk of postpartum depression.
How Should I Be Getting My DHA and Omega-3s?
Consuming DHA and EPA directly from foods and/or dietary supplements is the only practical way to obtain adequate levels of these fatty acids. ALA is a very common essential fatty acid found in many plant sources that can be converted to EPA and DHA in the body. However, the conversion is so limited that EPA and DHA must be consumed directly.
What does this mean? Plant sources of omega-3 fatty acids (ALA) will not do the trick.
Women can get omega-3 fatty acids from plant-based walnuts, flaxseeds, or chia seeds. However, since DHA is the critical form that moms need, plant-based sources that first must be converted into EPA and then into DHA will not be sufficient. Unfortunately, the conversion rate is too inefficient to give the pregnant body all that it needs. During pregnancy and while breastfeeding, experts recommend consuming 12 oz of fish/week and supplementing with at least 200 mg/day of DHA.
In terms of supplements, a combined pill of DHA/EPA is beneficial due to EPA's role in DHA absorption. EPA ensures that DHA reaches the placenta in sufficient amounts. High-quality fish oil is a reliable source for both DHA and EPA in supplement form. However, some studies have shown that the bioavailability of DHA from algal oil is equivalent to that from cooked salmon. Thus, algal oil is also a reliable DHA source. Lastly, some supplement providers do not include omega-3s in their prenatal vitamin since multiple ingredients may compromise the bioavailability of the fatty acids and make it difficult to obtain adequate amounts. It may be advisable to take a prenatal vitamin alongside a separate omega-3 pill.
How Much DHA Should I Be Taking During Pregnancy?
95% of childbearing-age women in the US don't consume enough DHA and EPA.
The recommended DHA supplemental dose will vary depending on how much fish you consume. During pregnancy, the total dietary goal for DHA is 300 mg/day minimum. Two servings of fish per week only provide about 50 to 100 mg of DHA. Plant-based sources found elsewhere in the diet supply insignificant amounts of EPA and DHA. Thus, the deficit should be corrected with fish oil supplements or algae-derived DHA supplements.
-
-
- Workshop on the Essentiality of and Recommended Dietary Intakes: 220 mg/day of DHA in adults; 300 mg/day of DHA in pregnant and lactating women
- World Health Organization: 200-500 mg/day of EPA + DHA
- Numerous Organizations: 450-500 mg/day of EPA/DHA (200-500 mg/day of EPA/DHA + 2 Servings of Fatty Fish)
-
What Are the Best Food and Dietary Sources of Omega-3 Fatty Acids? Is Eating Fish and Consuming Fish Oil Safe During Pregnancy?
Yes - seafood choices are encouraged during pregnancy!
The Environmental Protection Agency and The American College of Obstetricians and Gynecologists recommend that women consume 12 ounces of seafood per week from low-mercury species.
To avoid mercury toxicity, look for those sources that are higher in EPA and DHA and lower in methylmercury. These marine sources include:
- Salmon - Farmed salmon fed a diet of traditional marine ingredients is the best source of DHA/EPA.
- Sardines
- Anchovies
- Oysters (Pacific)
- Halibut
- Striped Bass
- Trout
- Tilapia
- Shrimp
- Crab
- Catfish/Flounder
- Roe (Fish Eggs)
You can also get small amounts of DHA in pasture-raised beef, chicken, and eggs. However, seafood has a much greater concentration of the essential fatty acid, DHA.
How Can I Get Omega-3s Without Eating Fish?
Plant sources of beneficial omega-3s, not DHA, include:
- Walnuts and walnut oil
- Brazil nuts
- Seeds (pumpkin, sunflower, chia, and flax)
Note: Intake of omega-6-rich oils found in sunflower, corn, and cottonseed oils should be minimized since they are converted into substrates that compete with EPA. Pregnant women should reduce their intake of these vegetable oils and substitute others rich in omega-3 fatty acids like flaxseed, canola, and soybean oil.
What About Mercury?
Certain fish are very high in mercury and should be avoided during pregnancy. Those fish include tuna, swordfish, tilefish, king mackerel, and shark. However, some canned tuna brands are promising low mercury levels. Even if your fish source contains a small amount of mercury, it also contains high amounts of selenium. This mineral readily binds with mercury, preventing it from exerting toxic effects in the body. Most importantly, fish provide many essential nutrients during pregnancy, besides our favorite DHA, including protein, iodine, zinc, and vitamin D. It would be a shame not to utilize fish, as the dietary nutritional powerhouse that it is, to nourish you and your baby during pregnancy!
How Can I Tell If I Am Getting Enough Omega-3s and DHA?
Not a popular test among physicians, omega-3 levels are best determined by looking at adipose tissue fatty acids for long-term intake and red blood cell fatty acids to reflect intake from the previous 120 days. Plasma fatty acid levels are thought to reflect more immediate intake. Thus, the type of blood test matters in determining your omega-3 levels.
EPA and DHA typically comprise about 3-5% of red blood cell fatty acids in Western populations with low fish intakes. In Japan, where fish consumption is high, red blood cell EPA and DHA levels are about twice those of Western populations.
Prenatal Vitamin Brands: What's the Omega-3/DHA Amount and Type in Popular Prenatal Brands?
| Name of the Prenatal | Amount | Type |
| Parsley Health Prenatal: Prenatal DHA Softgels separate from Parsley Prenatal: MaxSimil DHA Fish Oil Concentrate: | Total Omega-3 Fatty Acids 1.58 g |
DHA Docosahexaenoic Acid 1.35 g EPA Eicosapentaenoic Acid 236 mg |
| Modern Fertility Prenatal: | 100 mg | (Omega-3 Docosahexaenoic Acid (DHA) Fatty Acid from Schizeochytrium spp (microalgae)) |
| Ritual Prenatal: | 350 mg | (Omega-3 Docosahexaenoic Acid (DHA) Fatty Acid from Schizeochytrium spp (microalgae)) |
| FullWell Prenatal*: | None | N/A |
| Perelel: Conception Support and 1st Trimester Pack - Separate Capsule: | Total Omega 3 Fatty Acids 375 mg |
DHA (Docosahexaenoic Acid) and EPA (Eicosapentaenoic Acid) (250 mg DHA + 100 mg EPA) |
| NatureMade Prenatal Multi + DHA: | Total Omega-3 Fatty Acids from Fish Oil Concentrate 260 mg |
Omega-3 Docosahexaenoic Acid (DHA) 200 mg Omega-3 Eicosapentaenoic Acid (EPA) 60 mg |
| Seeking Health: Optimal Prenatal | None | N/A |
| Designs for Health: Prenatal Pro: | None | N/A |
*Fullwell believes the stability of the DHA is compromised when mixed into a multivitamin. They believe it is essential for a healthy pregnancy and should be taken separately with the prenatal. They also believe that there is a substantial benefit to taking DHA and EPA together.
Prenatal Analysis:
When looking at the prenatal vitaminl companies above, a small number of them directly include omega-3s in their prenatal vitamin. Many prenatal vitamins and supplements either do not contain omega-3s or are offered in a separate capsule. This is not to say that omega-3s are not critical to a healthy pregnancy; it emphasizes that how you supplement is important. Including a separate DHA pill in your prenatal supplement routine in the proper amount (300 mg/day) is ideal.
*Look for 3rd party independent testing to avoid contaminants in supplements.
Resources:
- Nichols L. Real Food for Pregnancy: The Science and Wisdom of Optimal Prenatal Nutrition. First edition. Lily Nichols; 2018.
- Preterm Birth Prevention: Omega-3 Fatty Acids. FullWell. Accessed February 11, 2022. https://fullwellfertility.com/blogs/blog/preterm-birth-prevention-omega-3-fatty-acids
- The Best Fish Oil Supplements for Pregnancy - Motherhood Community. Accessed February 11, 2022. https://motherhoodcommunity.com/these-are-the-best-fish-oil-supplement-for-pregnancy-everything-you-need-to-know/
- Murkoff HE, Mazel S. What to Expect When You’re Expecting. Fifth edition. Workman Publishing; 2016.
- Jacob A. Guest post: 6 Prenatal Nutrition Misconceptions That Need to Stop by Lily Nichols, RDN, CDE, CLT. Radicata Nutrition with Aglaée Jacob, MS Nutrition. Published February 15, 2015. Accessed February 11, 2022. https://radicatanutrition.com/guest-post-6-prenatal-nutrition-misconceptions-that-need-to-stop-by-lily-nichols-rdn-cde-clt/
- Is Docosahexaenoic Acid (DHA) Essential? Lessons from DHA Status Regulation, Our Ancient Diet, Epidemiology and Randomized Controlled Trials | The Journal of Nutrition | Oxford Academic. Accessed February 11, 2022. https://academic.oup.com/jn/article/134/1/183/4688233?login=false
- Shireman T, Kerling E, Gajewski B, Colombo J, Carlson S. Docosahexaenoic acid supplementation (DHA) and the return on investment for pregnancy outcomes13. Prostaglandins Leukot Essent Fatty Acids. 2016;111:8-10. doi:10.1016/j.plefa.2016.05.008
- Middleton P, Gomersall JC, Gould JF, Shepherd E, Olsen SF, Makrides M. Omega‐3 fatty acid addition during pregnancy. Cochrane Database Syst Rev. 2018;2018(11):CD003402. doi:10.1002/14651858.CD003402.pub3
- Nordgren TM, Lyden E, Anderson-Berry A, Hanson C. Omega-3 Fatty Acid Intake of Pregnant Women and Women of Childbearing Age in the United States: Potential for Deficiency? Nutrients. 2017;9(3):197. doi:10.3390/nu9030197
- Greenberg JA, Bell SJ, Ausdal WV. Omega-3 Fatty Acid Supplementation During Pregnancy. Rev Obstet Gynecol. 2008;1(4):162-169.
- Office of Dietary Supplements - Omega-3 Fatty Acids. Accessed February 11, 2022. https://ods.od.nih.gov/factsheets/Omega3FattyAcids-HealthProfessional/